Antibiotics stop working: WHO opens countdown

Medicines no longer heal. In just 30 years, the likelihood of dying from infection will be higher than from cancer or diabetes. Is there a chance to be saved
WHO is sounding the alarm: soon we will have nothing to treat. In less than 100 years since the discovery of penicillin, bacteria have managed to adapt to almost all existing antibiotics. The last significant invention was fluoroquinolones, and since then, humanity has begun to lose to microbes in the race for health.
The ability of microorganisms to survive and multiply while taking antibiotics is called antibiotic resistance. Simply put, bacteria began to respond to treatment as we do to rain. It’s unpleasant, but if you have an umbrella with you, it’s not scary. Pharmacologists know at least five ways in which microbes protect themselves from antibiotics. Some of them are innate features. Others are the result of exposure to small doses of drugs and the exchange of “beneficial” properties between different types of microorganisms.
Ideally, an antibiotic interrupts the microorganism’s multiplication chain at different stages. For example, it disrupts the synthesis of nucleic acids or the formation of the cell wall. Bacteria have learned to cope with this: someone actively throws out the active substance of the drug from the cell. Others disguise themselves or break down the antibiotic with special enzymes.
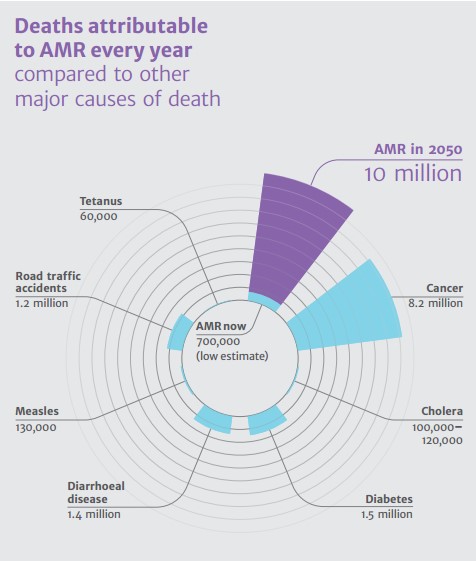
The statistics are relentless: if the situation is not changed, up to 10 million people will die from resistant strains of bacteria every year by 2050. This is more than deaths from cancer, road traffic accidents or diabetes. Already, treatment of multidrug-resistant tuberculosis is ineffective in almost half of the observations, and Russia is in the top three according to this diagnosis. Fighting microbes is sometimes still obtained by increasing doses and combining different drugs. But in 2015, microbes resistant to the last antibiotic of the reserve, colistin, appeared, and the world was on the verge of a post-antibiotic apocalypse.
British Review on Antimicrobial Resistance Prediction Promises A Throwback To The Middle Ages
Scientists are trying to find new ways to trick bacteria. The problem is that developing an antibiotic costs a lot of money, and a potentially powerful drug will be made a reserve drug and used only in extreme cases. This means that pharmaceutical companies will not “recoup” development costs. In addition, microbes can again be faster than humans and adapt to a new drug even before it hits the market.
However, there is occasional hope. For example, in August 2020, a weak spot was discovered in acinetobacter, the causative agent of respiratory diseases. Scientists conducted an experiment in which hydrogen sulphide made bacteria vulnerable to gentamicin.
The problem of antibiotic resistance is aggravated primarily by:
Taking uncontrolled antibiotics without a doctor’s prescription
Insufficient dosage or treatment time
Incorrect combination of drugs
At the same time, there is a possibility that the problem of antibiotic resistance will be relegated to the background. This will be the case when we learn to use antimicrobial peptides, bacteriophages, and gene modification of pathogens. While these ideas remain only within the walls of laboratories, our business is to protect ourselves from infections, to observe hygiene and doctor’s prescriptions.